If you’re a parent, you’ve probably experienced a few unexpected trips to an urgent care clinic to have your child’s aching ear or pink eye or sprained wrist treated. You may have even gone to the ER for more serious medical matters.
Pets sometimes need urgent or emergency care too.
However, there is a severe shortage of qualified veterinary staff, for several reasons:
Staffing shortages.
In this highly stressful profession, many staffers experience “compassion fatigue” and burnout. The mental and physical toll results in staffers leaving the profession, forcing clinics to cut back on hours or to close altogether.
Pandemic puppy boom.
One in five households across the U.S. added a dog or cat at the start of the COVID-19 pandemic, greatly surpassing the number of graduating veterinarians and putting extra strain on existing staff.
More pet owners.
The number of pet-owning households in the U.S. is increasing by 1.5% annually; the demand for pet health care services is increasing 6.1% annually.
Retirement.
More than 12,500 board-certified veterinarians are planning to retire by 2030.
The ever-increasing demand for veterinary services, combined with a severe shortage of qualified veterinary staff has resulted in many veterinary clinics and emergency hospitals turning away pet patients because they are at capacity.
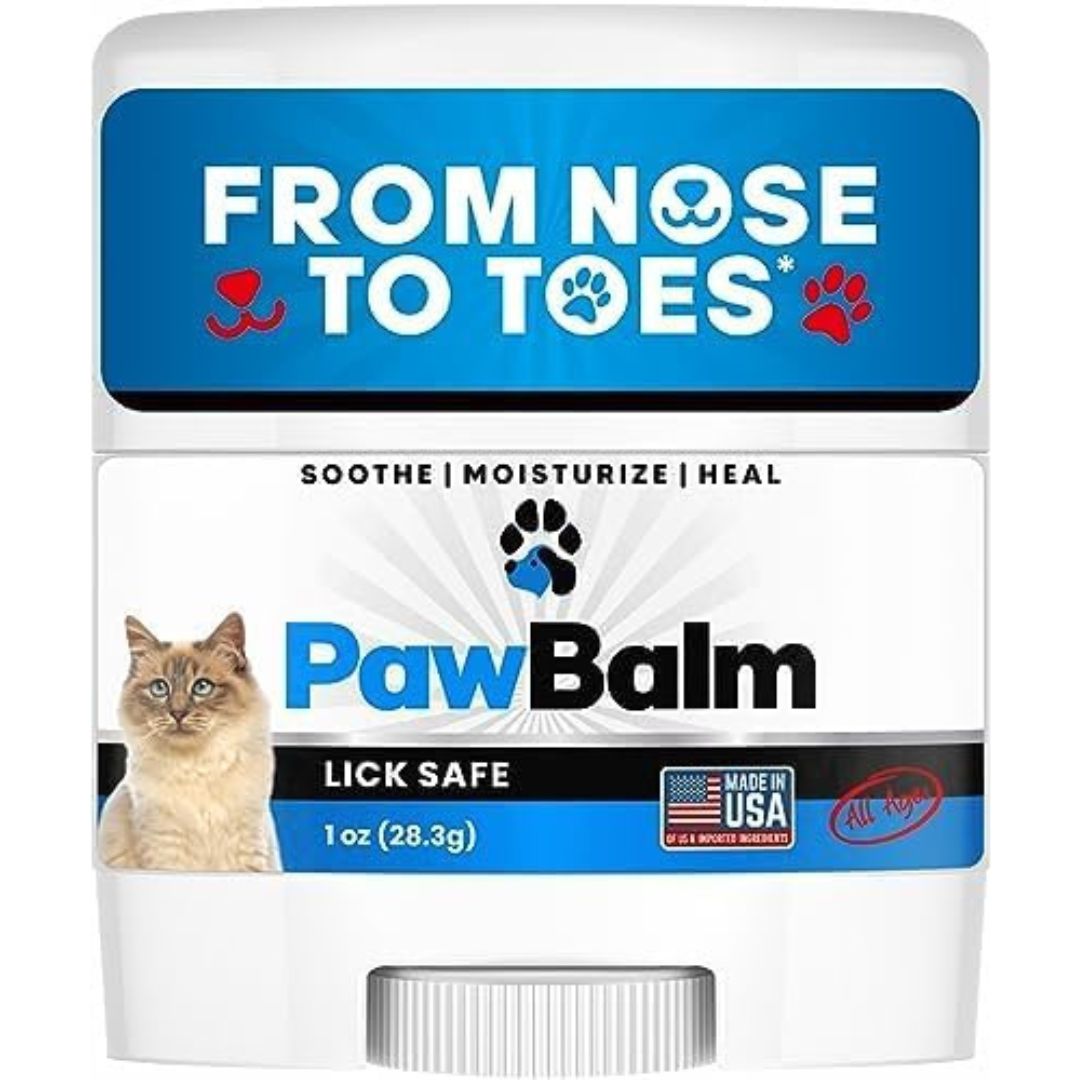
The ER Vets of Western Washington Facebook page regularly posts wait times for Emergency veterinarians. Here’s sampling of wait times during January 2024:
At Atlantic Veterinary Hospital, we try very hard to be there when you need us, but it requires creative scheduling, a willing staff, and a lot of hustle and hard work. By allowing room in our daily schedule for urgent and emergency care – with a slight fee increase – we help your pet get the immediate relief it needs and help you avoid a more costly visit and long waits at a veterinary emergency hospital.
Urgent Care Appointments
In addition to our regular pre-scheduled wellness and illness appointments, we reserve same-day Urgent Care appointments in our schedule every day.
There is a potential that these blocked-out appointments will not be filled, yet our staff needs to be on hand and prepared regardless.
Urgent medical conditions are uncomfortable, but not life-threatening, such as:
- Eyes – swelling, discharge, redness
- Ears – discharge, pain, odor, scratching, or shaking
- Coughing or sneezing
- Vomiting (minor or occasional)
- Diarrhea
- Mild constipation
- Change in urine color, frequency, or amount
- Straining to urinate, dribbling urine
- Change in amount of food or water intake
- Change in behavior (mild depression, anxiety, excessive sleepiness)
- Evidence of worms or fleas
- Minor wounds
- Lumps
- Facial swelling, licking, or scratching
Medical Emergencies
We also accept Emergencies to the best of our ability. Pets with life-threatening emergency conditions take precedence over all scheduled appointments.
The additional emergency fee helps cover our costs for working through breaks, lunches, calling in additional staff, and overtime costs. When we take in emergencies during the day, our staff members often must stay after hours to finish medical notes and return phone calls after hours.
Emergency medical conditions can include but are not limited to, conditions such as:
- Difficulty or irregular breathing
- Weakness or collapse
- Broken bones
- Severe trauma (hit by car, fall, gunshot wound, burns)
- Prolonged or multiple seizure
- Poison exposure
- Eating a foreign object
- Significant bleeding
- Paralysis
- High fever
- Significant wounds
- Repeated vomiting
- Inability to urinate or defecate
We Try Hard NOT to say “No”
Please know that if we have to say “No” to an established client requesting an Urgent or Emergency appointment, we have carefully considered our current patient load and tried to make it work, but have determined it would dangerously overwhelm the care of the patients we already have in the hospital with the staff we have available at that time.
We try very hard not to say “No.” Please do your part by communicating with us early if you think your pet is developing a medical condition that will require care.
Related articles:
Licensed Veterinary Nursing: A Recession-Proof Career that Combines a Love of Animals and People
Your Pet Shouldn’t Have to Wait to Feel Better! Consider Urgent Care